|
|
[Last Modified: ] |
 |
|
| [Plasmodium
falciparum] [Plasmodium malariae] [Plasmodium ovale] [Plasmodium vivax] |
Malaria antibody detection
can be performed using various techniques. For the clinical laboratory, the most
practical approach is the indirect fluorescent antibody (IFA) test. This test, with
malaria parasites as antigens, detects most sensitively antibody responses to a wide range
of plasmodial antigens.
The IFA procedure can be used to determine if a patient has been infected with Plasmodium. Because of the time required for development of antibody and also the persistence
of antibodies, serologic testing is not practical for routine diagnosis of malaria.
However, serology may be useful for:
- screening blood donors involved in cases of transfusion-induced malaria when the donor's parasitemia may be below the detectable level of blood film examination
- testing a patient with a febrile illness who is suspected of having malaria and from whom repeated blood smears are negative
Species-specific testing is available for the four human species: P. falciparum, P. vivax, P. malariae, and P. ovale. Cross-reactions often occur between Plasmodium species and Babesia species. Blood stage Plasmodium species schizonts (meronts) are used as antigen. The patient's serum is exposed to the organisms; homologous antibody, if present, attaches to the antigen, forming an antigen-antibody (Ag-Ab) complex. Fluorescein-labeled antihuman antibody is then added, which attaches to the patient's malaria-specific antibody. When examined with a fluorescence microscope, a positive reaction is when the parasites appear fluorescent yellow.
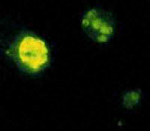 |
| A |
A: Positive malaria IFA showing a fluorescent schizont.
Reference:
Sulzer AJ,Wilson M. The fluorescent antibody test for malaria. Crit Rev Clin Lab Sci 1971;2:601-609.
|
|||